Framingham Risk Score Calculator Pdf To Jpg
- SCORE Risk charts SCORE Memo Card. The interactive tool for predicting and managing the risk of heart. Assessing Cardiovascular Risk: Systematic Evidence Review from the Risk Assessment Work Group. Risk Calculator; Background. Framingham Coronary Heart Disease Risk Score.
- Using 10-year CVD risk from Step 2, determine if patient is Low, Moderate or High risk.† Indicate Lipid and/or Apo B targets Step 31 Using the total points from Step 1, determine heart age (in years). 1 Adapted from: D’Agostino RB et al.(i). General cardiovascular risk profile for use in primary care. The Framingham Heart Study. Circ 2008;117:743-53.
- Framingham Risk Calculator
- Framingham Risk Score Calculator Pdf To Jpg Converter
- Framingham Risk Calculator Pda
- Framingham Risk Score Calculator Download
This ASCVD Risk Calculator is a companion tool to the 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk. Models included the Framingham-based ATP-III model, 1 the Reynolds Risk Score, and the Framingham CVD model. 6 The published ATP-III model was poorly calibrated for CHD, and the Reynolds Risk Score was better calibrated for major CVD than the Framingham CVD model. Moreover, after recalibration, the Reynolds Risk Score continued to show.
Abstract
For the primary prevention of cardiovascular disease, the Framingham Risk Score (FRS) is the most well-known risk prediction method. However, there are limited data regarding physicians' method of risk assessment and guideline adherence in clinical practice.
In the PARADIGM (Primary cARe AuDIt of Global risk Management) study (March 2009–10), 105 primary care physicians across Canada prospectively collected data for 3015 patients (mean age 56 years, 59% men) without known cardiovascular disease, diabetes, or lipid-lowering medications at baseline. For each patient, the treating physician determined their cardiovascular risk, and reported the risk stratification method and subsequent treatment decisions. Kappa statistics assessed the agreement between the study-calculated FRS and the treating physician's reported risk assessment. The FRS was the most commonly reported risk assessment method, but was used in only 34.0% of patients. Regardless of the method used (even if the FRS was reportedly used), there was only fair agreement between the risk stratification as reported by the physician and the study-calculated FRS. Moreover, physicians recommended statin initiation in 92% of all patients that they identified as high risk; however, according to the study-calculated FRS, only 56% of the truly high-risk patients were recommended statin therapy.
For the primary prevention of cardiovascular disease, these findings indicate a need to improve risk assessment and stratification, as misclassification directly contributes to suboptimal risk factor management in real-world clinical practice. Future studies should establish the optimal risk stratification method with quality improvement strategies for its subsequent implementation.
http://clinicaltrials.gov/ct2/show/NCT00950703; NCT00950703.
Introduction
In 2009, over 68 000 deaths in Canada were attributed to major cardiovascular diseases.1 While this remains high, appropriate risk assessment and risk factor management have resulted in a significant reduction of cardiovascular morbidity and mortality in Canada.2,3
Risk prediction tools4–7 can identify patients most likely to benefit from intervention, thereby guiding management decisions. Although the Framingham Risk Score (FRS) is the most well-known risk prediction method for the primary prevention of cardiovascular disease, other objective risk assessment options include the Reynold's Risk Score (RRS), high-sensitivity C-reactive protein, total number of risk factors, and carotid ultrasound to detect atherosclerosis.8 Alternately, physicians may use their overall subjective clinical assessment to estimate risk and guide management decisions.
Previous studies in acute coronary syndromes (ACSs) have described the discrepancies between objective and subjective global risk assessment.9–12 These discrepancies may contribute to important care gaps such as suboptimal treatment regimens and failure to reach guideline-recommended targets, and therefore suboptimal outcomes.9–12 Whether such discrepancies in risk assessment and guideline adherence exist in the primary prevention of cardiovascular disease in ‘real-world’ clinical practice is currently unknown.
In this observational study, we used data from the PARADIGM (Primary cAReAuDIt of Global risk Management) study to: (i) examine primary care physician assessment of cardiovascular risk in patients without known cardiovascular disease; (ii) evaluate the level of agreement of risk assessment between treating physicians and the FRS; and (iii) compare actual practice with established guidelines.
Methods
Setting
The PARADIGM study was a multicentre, prospective study that occurred between March 2009 and March 2010. It was approved by a central ethics review board (IRB Services). Primary care physicians whose practices included the management of patients for the primary prevention of cardiovascular disease (as assumed by their high statin prescribing patterns) were recruited to participate in the study.
Patients
From 10 provinces across Canada, 105 treating physician investigators consented and enrolled 3015 eligible patients into the study. Investigators prospectively collected and reported data using a standardized case report form. The inclusion criteria were asymptomatic, non-diabetic men (≥40 years), or women (≥50 years), who were seen in the office within the last year for a cardiovascular risk assessment. The exclusion criteria were history of diabetes or atherosclerosis (i.e. myocardial infarction, stroke, peripheral arterial disease, angina, or transient ischaemic attack), active liver disease or hepatic dysfunction (ALT >2 × upper limit of normal), active renal disease (baseline creatinine >170 µmol/L), history of malignancy within the past 5 years, chronic inflammatory conditions (i.e. arthritis, lupus, and inflammatory bowel disease), and known alcohol or drug abuse. Patients who had prior or current use of lipid-lowering therapies (statins, ezetimibe, fibrates, niacin, and fish oil), postmenopausal hormone replacement therapy, immunosuppressive medications, or oral steroids were also excluded. Patients who were known to have a high baseline cardiovascular risk (high risk by an FRS) were also excluded.
Main measurements
The case report form recorded data on demographics, medical history, medication use, and physical examination (such as anthropometric measurements and blood pressure). Laboratory investigations were performed within 6 weeks of the initial visit. At the second visit (<60 days after the initial visit), the treating physician re-assessed the patient and reported the patient's global cardiovascular risk as either low, intermediate, or high risk. Additionally, the physician recorded their choice of risk assessment method, and if applicable, the choice of drug therapy (for lipid or blood pressure management).
Study design
Continuous variables are presented as median (interquartile ranges) and compared by the Mann–Whitney U test. Categorical variables are presented as percentages and compared by the χ2 test. Guideline comparisons were made with the contemporary 2009 Canadian Cardiovascular Society (CCS)7 dyslipidemia guidelines, given that PARADIGM preceded the most recent 2012 CCS guidelines.6 Because the FRS is the most common risk stratification method and is also supported by the CCS, we used the recorded baseline data to formally calculate the 2008 FRS13 for a 10-year risk of cardiovascular disease (henceforth termed ‘study-calculated FRS’), as recommended in the 2009 CCS dyslipidemia guidelines. The study-calculated FRS was compared with the risk assessment reported by the treating physician. Kappa scores were used to assess the degree of agreement beyond chance: 0 (none), 0–0.2 (slight), 0.2–0.4 (fair), 0.4–0.6 (moderate), 0.6–0.8 (substantial), and 0.8–1.0 (almost perfect). Data analysis was performed using SPSS 21.0 (IBM), and P-values of <0.05 were considered to be statistically significant.
Results
In total, 3015 patients were enrolled in 2009–10. Table 1 summarizes their baseline characteristics, as stratified by the investigators' reported cardiovascular risk assessment of low (n = 1532), intermediate (n = 1093), or high (n = 390) risk. Patients reported to be at high risk were more likely to be male and older, with higher systolic blood pressures and LDL levels. At baseline, patients classified in the high-risk category were also more likely to be taking aspirin, angiotensin-converting enzyme inhibitors, calcium channel blockers, and diuretics.
Baseline patient characteristics
Overall (n = 3015)| Risk-stratified by physician | P-value for trend | ||||
|---|---|---|---|---|---|
| Low risk (n = 1532) | Intermediate risk (n = 1093) | High risk (n = 390) | |||
| Age (years)a | 56.3 | 54 (50–60) | 57 (52–63) | 58 (52–65) | |
| Male, n (%) | 1774 | 811 (52.9%) | 701 (64.1%) | 262 (67.2%) | |
| Ethnicity | |||||
| European, n (%) | 2099 (69.6%) | 971 (46.3%) | 813 (38.7%) | 315 (15.0%) | <0.001 |
| Chinese, n (%) | 266 (8.8%) | 194 (72.9%) | 61 (22.9%) | 11 (4.1%) | |
| Other Asian, n (%) | 241 (8.0%) | 172 (71.4%) | 60 (24.9%) | 9 (3.7%) | |
| South Asian, n (%) | 250 (8.3%) | 112 (44.8%) | 105 (42.0%) | 33 (13.2%) | |
| Other, n (%) | 88 (2.9%) | 44 (50.0%) | 31 (35.2%) | 13 (14.8%) | |
| African, n (%) | 71 (2.4%) | 39 (54.9%) | 23 (32.4%) | 9 (12.7%) | |
| Co-morbidities | |||||
| Hypertension, n (%) | 917 (30.4%) | 332 (21.7%) | 416 (38.1%) | 169 (43.3%) | <0.001 |
| Treated hypertension, n (%) | 803 (26.6%) | 289 (18.9%) | 367 (33.6%) | 147 (37.7%) | <0.001 |
| History of smoking, n (%) | 1046 (34.7%) | 410 (26.8%) | 429 (39.2%) | 207 (53.1%) | <0.001 |
| First degree relative with vascular disease <60 years old, n (%) | 732 (24.3%) | 296 (19.4%) | 307 (28.1%) | 129 (33.2%) | <0.001 |
| Health measurements | |||||
| Systolic blood pressure (mmHg)a | 126.6 ± 14.0 | 122 (113–130) | 130 (120–137) | 130 (122–140) | <0.001 |
| Diastolic blood pressure (mmHg)a | 78.5 ± 9.1 | 80 (70–82) | 80 (74–85) | 80 (73–86) | <0.001 |
| Weight (kg)b | 79.2 ± 18.2 | 74.5 ± 17.0 | 82.7 ± 17.5 | 87.8 ± 19.0 | <0.001 |
| Waist circumference (cm)b | 94.8 ± 13.6 | 91 ± 13 | 98 ± 12 | 102 ± 14 | <0.001 |
| BMI (kg/m2)b | 27.81 ± 5.32 | 26.4 ± 4.6 | 28.7 ± 5.2 | 30.5 ± 5.7 | <0.001 |
| LDL-C (mmol/L)b | 3.6 ± 0.8 | 3.40 ± 0.78 | 3.72 ± 0.82 | 3.80 ± 0.97 | <0.001 |
| HDL-C (mmol/L)b | 1.4 ± 0.4 | 1.47 ± 0.41 | 1.32 ± 0.36 | 1.22 ± 0.34 | <0.001 |
| Total cholesterol (mmol/L)b | 5.6 ± 1.0 | 5.46 ± 0.90 | 5.79 ± 0.98 | 5.93 ± 1.14 | <0.001 |
| Triglyceride (mmol/L)b | 1.6 ± 1.0 | 1.34 ± 0.76 | 1.71 ± 1.16 | 2.06 ± 1.36 | <0.001 |
| Fasting blood glucose (mmol/L)b | 5.4 ± 0.7 | 5.25 ± 0.62 | 5.43 ± 0.66 | 5.66 ± 1.11 | <0.001 |
| HbA1c (%)b | 5.7 ± 0.5 | 5.7 ± 0.4 | 5.7 ± 0.4 | 5.7 ± 0.7 | <0.001 |
| Creatinine (µmol/L)b | 80.0 ± 16.1 | 78 ± 15 | 82 ± 16 | 84 ± 17 | <0.001 |
| eGFR (mL/min/1.73 m2)b | 77.4 ± 16.0 | 80.2 ± 16.1 | 75.4 ± 15.0 | 71.9 ± 16.0 | <0.001 |
| hsCRP (mg/L)b | 2.6 ± 3.2 | 1.96 ± 3.17 | 3.45 ± 4.85 | 5.40 ± 4.86 | <0.001 |
| Medication use at baseline visit | |||||
| Aspirin | 406 (13.5%) | 139 (9.1%) | 194 (17.7%) | 73 (18.7%) | <0.001 |
| ACE inhibitor | 327 (10.8%) | 115 (7.5%) | 151 (13.8%) | 61 (15.6%) | <0.001 |
| Angiotension receptor blocker | 333 (11.0%) | 109 (7.1%) | 165 (15.1%) | 59 (15.1%) | <0.001 |
| Beta-blocker | 120 (4.0%) | 49 (3.2%) | 49 (4.5%) | 22 (5.6%) | 0.014 |
| Direct renin inhibitor | 13 (0.4%) | 2 (0.1%) | 6 (0.5%) | 5 (1.3%) | 0.002 |
| Calcium channel blocker | 166 (5.5%) | 59 (3.9%) | 64 (5.9%) | 43 (11.0%) | <0.001 |
| Diuretic | 444 (14.7%) | 148 (9.7%) | 200 (18.3%) | 96 (24.6%) | <0.001 |
| Risk-stratified by physician | P-value for trend | ||||
|---|---|---|---|---|---|
| Low risk (n = 1532) | Intermediate risk (n = 1093) | High risk (n = 390) | |||
| Age (years)a | 56.3 | 54 (50–60) | 57 (52–63) | 58 (52–65) | |
| Male, n (%) | 1774 | 811 (52.9%) | 701 (64.1%) | 262 (67.2%) | |
| Ethnicity | |||||
| European, n (%) | 2099 (69.6%) | 971 (46.3%) | 813 (38.7%) | 315 (15.0%) | <0.001 |
| Chinese, n (%) | 266 (8.8%) | 194 (72.9%) | 61 (22.9%) | 11 (4.1%) | |
| Other Asian, n (%) | 241 (8.0%) | 172 (71.4%) | 60 (24.9%) | 9 (3.7%) | |
| South Asian, n (%) | 250 (8.3%) | 112 (44.8%) | 105 (42.0%) | 33 (13.2%) | |
| Other, n (%) | 88 (2.9%) | 44 (50.0%) | 31 (35.2%) | 13 (14.8%) | |
| African, n (%) | 71 (2.4%) | 39 (54.9%) | 23 (32.4%) | 9 (12.7%) | |
| Co-morbidities | |||||
| Hypertension, n (%) | 917 (30.4%) | 332 (21.7%) | 416 (38.1%) | 169 (43.3%) | <0.001 |
| Treated hypertension, n (%) | 803 (26.6%) | 289 (18.9%) | 367 (33.6%) | 147 (37.7%) | <0.001 |
| History of smoking, n (%) | 1046 (34.7%) | 410 (26.8%) | 429 (39.2%) | 207 (53.1%) | <0.001 |
| First degree relative with vascular disease <60 years old, n (%) | 732 (24.3%) | 296 (19.4%) | 307 (28.1%) | 129 (33.2%) | <0.001 |
| Health measurements | |||||
| Systolic blood pressure (mmHg)a | 126.6 ± 14.0 | 122 (113–130) | 130 (120–137) | 130 (122–140) | <0.001 |
| Diastolic blood pressure (mmHg)a | 78.5 ± 9.1 | 80 (70–82) | 80 (74–85) | 80 (73–86) | <0.001 |
| Weight (kg)b | 79.2 ± 18.2 | 74.5 ± 17.0 | 82.7 ± 17.5 | 87.8 ± 19.0 | <0.001 |
| Waist circumference (cm)b | 94.8 ± 13.6 | 91 ± 13 | 98 ± 12 | 102 ± 14 | <0.001 |
| BMI (kg/m2)b | 27.81 ± 5.32 | 26.4 ± 4.6 | 28.7 ± 5.2 | 30.5 ± 5.7 | <0.001 |
| LDL-C (mmol/L)b | 3.6 ± 0.8 | 3.40 ± 0.78 | 3.72 ± 0.82 | 3.80 ± 0.97 | <0.001 |
| HDL-C (mmol/L)b | 1.4 ± 0.4 | 1.47 ± 0.41 | 1.32 ± 0.36 | 1.22 ± 0.34 | <0.001 |
| Total cholesterol (mmol/L)b | 5.6 ± 1.0 | 5.46 ± 0.90 | 5.79 ± 0.98 | 5.93 ± 1.14 | <0.001 |
| Triglyceride (mmol/L)b | 1.6 ± 1.0 | 1.34 ± 0.76 | 1.71 ± 1.16 | 2.06 ± 1.36 | <0.001 |
| Fasting blood glucose (mmol/L)b | 5.4 ± 0.7 | 5.25 ± 0.62 | 5.43 ± 0.66 | 5.66 ± 1.11 | <0.001 |
| HbA1c (%)b | 5.7 ± 0.5 | 5.7 ± 0.4 | 5.7 ± 0.4 | 5.7 ± 0.7 | <0.001 |
| Creatinine (µmol/L)b | 80.0 ± 16.1 | 78 ± 15 | 82 ± 16 | 84 ± 17 | <0.001 |
| eGFR (mL/min/1.73 m2)b | 77.4 ± 16.0 | 80.2 ± 16.1 | 75.4 ± 15.0 | 71.9 ± 16.0 | <0.001 |
| hsCRP (mg/L)b | 2.6 ± 3.2 | 1.96 ± 3.17 | 3.45 ± 4.85 | 5.40 ± 4.86 | <0.001 |
| Medication use at baseline visit | |||||
| Aspirin | 406 (13.5%) | 139 (9.1%) | 194 (17.7%) | 73 (18.7%) | <0.001 |
| ACE inhibitor | 327 (10.8%) | 115 (7.5%) | 151 (13.8%) | 61 (15.6%) | <0.001 |
| Angiotension receptor blocker | 333 (11.0%) | 109 (7.1%) | 165 (15.1%) | 59 (15.1%) | <0.001 |
| Beta-blocker | 120 (4.0%) | 49 (3.2%) | 49 (4.5%) | 22 (5.6%) | 0.014 |
| Direct renin inhibitor | 13 (0.4%) | 2 (0.1%) | 6 (0.5%) | 5 (1.3%) | 0.002 |
| Calcium channel blocker | 166 (5.5%) | 59 (3.9%) | 64 (5.9%) | 43 (11.0%) | <0.001 |
| Diuretic | 444 (14.7%) | 148 (9.7%) | 200 (18.3%) | 96 (24.6%) | <0.001 |
hsCRP, high-sensitivity C-reactive protein; eGFR, estimated glomerular filtration rate; ACE, angiotensin-converting enzyme.
Baseline patient characteristics
Overall (n = 3015)| Risk-stratified by physician | P-value for trend | ||||
|---|---|---|---|---|---|
| Low risk (n = 1532) | Intermediate risk (n = 1093) | High risk (n = 390) | |||
| Age (years)a | 56.3 | 54 (50–60) | 57 (52–63) | 58 (52–65) | |
| Male, n (%) | 1774 | 811 (52.9%) | 701 (64.1%) | 262 (67.2%) | |
| Ethnicity | |||||
| European, n (%) | 2099 (69.6%) | 971 (46.3%) | 813 (38.7%) | 315 (15.0%) | <0.001 |
| Chinese, n (%) | 266 (8.8%) | 194 (72.9%) | 61 (22.9%) | 11 (4.1%) | |
| Other Asian, n (%) | 241 (8.0%) | 172 (71.4%) | 60 (24.9%) | 9 (3.7%) | |
| South Asian, n (%) | 250 (8.3%) | 112 (44.8%) | 105 (42.0%) | 33 (13.2%) | |
| Other, n (%) | 88 (2.9%) | 44 (50.0%) | 31 (35.2%) | 13 (14.8%) | |
| African, n (%) | 71 (2.4%) | 39 (54.9%) | 23 (32.4%) | 9 (12.7%) | |
| Co-morbidities | |||||
| Hypertension, n (%) | 917 (30.4%) | 332 (21.7%) | 416 (38.1%) | 169 (43.3%) | <0.001 |
| Treated hypertension, n (%) | 803 (26.6%) | 289 (18.9%) | 367 (33.6%) | 147 (37.7%) | <0.001 |
| History of smoking, n (%) | 1046 (34.7%) | 410 (26.8%) | 429 (39.2%) | 207 (53.1%) | <0.001 |
| First degree relative with vascular disease <60 years old, n (%) | 732 (24.3%) | 296 (19.4%) | 307 (28.1%) | 129 (33.2%) | <0.001 |
| Health measurements | |||||
| Systolic blood pressure (mmHg)a | 126.6 ± 14.0 | 122 (113–130) | 130 (120–137) | 130 (122–140) | <0.001 |
| Diastolic blood pressure (mmHg)a | 78.5 ± 9.1 | 80 (70–82) | 80 (74–85) | 80 (73–86) | <0.001 |
| Weight (kg)b | 79.2 ± 18.2 | 74.5 ± 17.0 | 82.7 ± 17.5 | 87.8 ± 19.0 | <0.001 |
| Waist circumference (cm)b | 94.8 ± 13.6 | 91 ± 13 | 98 ± 12 | 102 ± 14 | <0.001 |
| BMI (kg/m2)b | 27.81 ± 5.32 | 26.4 ± 4.6 | 28.7 ± 5.2 | 30.5 ± 5.7 | <0.001 |
| LDL-C (mmol/L)b | 3.6 ± 0.8 | 3.40 ± 0.78 | 3.72 ± 0.82 | 3.80 ± 0.97 | <0.001 |
| HDL-C (mmol/L)b | 1.4 ± 0.4 | 1.47 ± 0.41 | 1.32 ± 0.36 | 1.22 ± 0.34 | <0.001 |
| Total cholesterol (mmol/L)b | 5.6 ± 1.0 | 5.46 ± 0.90 | 5.79 ± 0.98 | 5.93 ± 1.14 | <0.001 |
| Triglyceride (mmol/L)b | 1.6 ± 1.0 | 1.34 ± 0.76 | 1.71 ± 1.16 | 2.06 ± 1.36 | <0.001 |
| Fasting blood glucose (mmol/L)b | 5.4 ± 0.7 | 5.25 ± 0.62 | 5.43 ± 0.66 | 5.66 ± 1.11 | <0.001 |
| HbA1c (%)b | 5.7 ± 0.5 | 5.7 ± 0.4 | 5.7 ± 0.4 | 5.7 ± 0.7 | <0.001 |
| Creatinine (µmol/L)b | 80.0 ± 16.1 | 78 ± 15 | 82 ± 16 | 84 ± 17 | <0.001 |
| eGFR (mL/min/1.73 m2)b | 77.4 ± 16.0 | 80.2 ± 16.1 | 75.4 ± 15.0 | 71.9 ± 16.0 | <0.001 |
| hsCRP (mg/L)b | 2.6 ± 3.2 | 1.96 ± 3.17 | 3.45 ± 4.85 | 5.40 ± 4.86 | <0.001 |
| Medication use at baseline visit | |||||
| Aspirin | 406 (13.5%) | 139 (9.1%) | 194 (17.7%) | 73 (18.7%) | <0.001 |
| ACE inhibitor | 327 (10.8%) | 115 (7.5%) | 151 (13.8%) | 61 (15.6%) | <0.001 |
| Angiotension receptor blocker | 333 (11.0%) | 109 (7.1%) | 165 (15.1%) | 59 (15.1%) | <0.001 |
| Beta-blocker | 120 (4.0%) | 49 (3.2%) | 49 (4.5%) | 22 (5.6%) | 0.014 |
| Direct renin inhibitor | 13 (0.4%) | 2 (0.1%) | 6 (0.5%) | 5 (1.3%) | 0.002 |
| Calcium channel blocker | 166 (5.5%) | 59 (3.9%) | 64 (5.9%) | 43 (11.0%) | <0.001 |
| Diuretic | 444 (14.7%) | 148 (9.7%) | 200 (18.3%) | 96 (24.6%) | <0.001 |
| Risk-stratified by physician | P-value for trend | ||||
|---|---|---|---|---|---|
| Low risk (n = 1532) | Intermediate risk (n = 1093) | High risk (n = 390) | |||
| Age (years)a | 56.3 | 54 (50–60) | 57 (52–63) | 58 (52–65) | |
| Male, n (%) | 1774 | 811 (52.9%) | 701 (64.1%) | 262 (67.2%) | |
| Ethnicity | |||||
| European, n (%) | 2099 (69.6%) | 971 (46.3%) | 813 (38.7%) | 315 (15.0%) | <0.001 |
| Chinese, n (%) | 266 (8.8%) | 194 (72.9%) | 61 (22.9%) | 11 (4.1%) | |
| Other Asian, n (%) | 241 (8.0%) | 172 (71.4%) | 60 (24.9%) | 9 (3.7%) | |
| South Asian, n (%) | 250 (8.3%) | 112 (44.8%) | 105 (42.0%) | 33 (13.2%) | |
| Other, n (%) | 88 (2.9%) | 44 (50.0%) | 31 (35.2%) | 13 (14.8%) | |
| African, n (%) | 71 (2.4%) | 39 (54.9%) | 23 (32.4%) | 9 (12.7%) | |
| Co-morbidities | |||||
| Hypertension, n (%) | 917 (30.4%) | 332 (21.7%) | 416 (38.1%) | 169 (43.3%) | <0.001 |
| Treated hypertension, n (%) | 803 (26.6%) | 289 (18.9%) | 367 (33.6%) | 147 (37.7%) | <0.001 |
| History of smoking, n (%) | 1046 (34.7%) | 410 (26.8%) | 429 (39.2%) | 207 (53.1%) | <0.001 |
| First degree relative with vascular disease <60 years old, n (%) | 732 (24.3%) | 296 (19.4%) | 307 (28.1%) | 129 (33.2%) | <0.001 |
| Health measurements | |||||
| Systolic blood pressure (mmHg)a | 126.6 ± 14.0 | 122 (113–130) | 130 (120–137) | 130 (122–140) | <0.001 |
| Diastolic blood pressure (mmHg)a | 78.5 ± 9.1 | 80 (70–82) | 80 (74–85) | 80 (73–86) | <0.001 |
| Weight (kg)b | 79.2 ± 18.2 | 74.5 ± 17.0 | 82.7 ± 17.5 | 87.8 ± 19.0 | <0.001 |
| Waist circumference (cm)b | 94.8 ± 13.6 | 91 ± 13 | 98 ± 12 | 102 ± 14 | <0.001 |
| BMI (kg/m2)b | 27.81 ± 5.32 | 26.4 ± 4.6 | 28.7 ± 5.2 | 30.5 ± 5.7 | <0.001 |
| LDL-C (mmol/L)b | 3.6 ± 0.8 | 3.40 ± 0.78 | 3.72 ± 0.82 | 3.80 ± 0.97 | <0.001 |
| HDL-C (mmol/L)b | 1.4 ± 0.4 | 1.47 ± 0.41 | 1.32 ± 0.36 | 1.22 ± 0.34 | <0.001 |
| Total cholesterol (mmol/L)b | 5.6 ± 1.0 | 5.46 ± 0.90 | 5.79 ± 0.98 | 5.93 ± 1.14 | <0.001 |
| Triglyceride (mmol/L)b | 1.6 ± 1.0 | 1.34 ± 0.76 | 1.71 ± 1.16 | 2.06 ± 1.36 | <0.001 |
| Fasting blood glucose (mmol/L)b | 5.4 ± 0.7 | 5.25 ± 0.62 | 5.43 ± 0.66 | 5.66 ± 1.11 | <0.001 |
| HbA1c (%)b | 5.7 ± 0.5 | 5.7 ± 0.4 | 5.7 ± 0.4 | 5.7 ± 0.7 | <0.001 |
| Creatinine (µmol/L)b | 80.0 ± 16.1 | 78 ± 15 | 82 ± 16 | 84 ± 17 | <0.001 |
| eGFR (mL/min/1.73 m2)b | 77.4 ± 16.0 | 80.2 ± 16.1 | 75.4 ± 15.0 | 71.9 ± 16.0 | <0.001 |
| hsCRP (mg/L)b | 2.6 ± 3.2 | 1.96 ± 3.17 | 3.45 ± 4.85 | 5.40 ± 4.86 | <0.001 |
| Medication use at baseline visit | |||||
| Aspirin | 406 (13.5%) | 139 (9.1%) | 194 (17.7%) | 73 (18.7%) | <0.001 |
| ACE inhibitor | 327 (10.8%) | 115 (7.5%) | 151 (13.8%) | 61 (15.6%) | <0.001 |
| Angiotension receptor blocker | 333 (11.0%) | 109 (7.1%) | 165 (15.1%) | 59 (15.1%) | <0.001 |
| Beta-blocker | 120 (4.0%) | 49 (3.2%) | 49 (4.5%) | 22 (5.6%) | 0.014 |
| Direct renin inhibitor | 13 (0.4%) | 2 (0.1%) | 6 (0.5%) | 5 (1.3%) | 0.002 |
| Calcium channel blocker | 166 (5.5%) | 59 (3.9%) | 64 (5.9%) | 43 (11.0%) | <0.001 |
| Diuretic | 444 (14.7%) | 148 (9.7%) | 200 (18.3%) | 96 (24.6%) | <0.001 |
hsCRP, high-sensitivity C-reactive protein; eGFR, estimated glomerular filtration rate; ACE, angiotensin-converting enzyme.
In comparison with the physician-determined level of risk, as demonstrated in Table 2, the study-calculated FRS classified more patients as high risk (n = 679), whereas fewer patients were classified as low (n = 1314) or intermediate risk (n = 1021). Specifically, physicians identified 12.9% of all patients as high risk, whereas the study-calculated FRS classified 22.5% of all patients as high risk.
Physician-reported risk assessment vs. study-calculated FRS for all patients
Study-calculated FRS stratification| Low | Intermediate | High | Total | |
|---|---|---|---|---|
| Physician-reported risk stratification | ||||
| Low | 947 | 446 | 138 | 1531 |
| Intermediate | 299 | 452 | 342 | 1093 |
| High | 68 | 123 | 199 | 390 |
| Total | 1314 | 1021 | 679 | 3014 |
| Low | Intermediate | High | Total | |
|---|---|---|---|---|
| Physician-reported risk stratification | ||||
| Low | 947 | 446 | 138 | 1531 |
| Intermediate | 299 | 452 | 342 | 1093 |
| High | 68 | 123 | 199 | 390 |
| Total | 1314 | 1021 | 679 | 3014 |
Physician-reported risk assessment vs. study-calculated FRS for all patients
Study-calculated FRS stratification| Low | Intermediate | High | Total | |
|---|---|---|---|---|
| Physician-reported risk stratification | ||||
| Low | 947 | 446 | 138 | 1531 |
| Intermediate | 299 | 452 | 342 | 1093 |
| High | 68 | 123 | 199 | 390 |
| Total | 1314 | 1021 | 679 | 3014 |
| Low | Intermediate | High | Total | |
|---|---|---|---|---|
| Physician-reported risk stratification | ||||
| Low | 947 | 446 | 138 | 1531 |
| Intermediate | 299 | 452 | 342 | 1093 |
| High | 68 | 123 | 199 | 390 |
| Total | 1314 | 1021 | 679 | 3014 |
Figure 1 presents the method of cardiovascular risk assessment as reported by the treating physician. Approximately one-third of patients were stratified via the FRS, while subjective clinical judgement was used to stratify another third of patients, and alternative methods were applied for the remaining third.
Physician-reported risk assessment method (n = 3015).
Physician-reported risk assessment method (n = 3015).
In Tables 2–4, kappa scores are used to illustrate the level of agreement between the study-calculated FRS and the physician's estimate of cardiovascular risk. For all patients (n = 3014), the overall agreement between the study-calculated FRS and physician-estimated risk was only fair (kappa score 0.25). Similarly, when the treating physicians reported using a risk stratification method other than FRS (n = 1988), the kappa score was 0.22 (fair agreement). However, even when the treating physicians reported using the FRS (n = 1026), the kappa score was only 0.31 (fair agreement) when compared with the study-calculated FRS.
Physician-reported (non-FRS) vs. study-calculated FRS
Study-calculated FRS stratification| Low | Intermediate | High | Total | |
|---|---|---|---|---|
| Physician-reported risk stratification | ||||
| Low | 570 | 250 | 86 | 906 |
| Intermediate | 256 | 312 | 215 | 783 |
| High | 66 | 103 | 130 | 299 |
| Total | 892 | 665 | 431 | 1988 |
| Low | Intermediate | High | Total | |
|---|---|---|---|---|
| Physician-reported risk stratification | ||||
| Low | 570 | 250 | 86 | 906 |
| Intermediate | 256 | 312 | 215 | 783 |
| High | 66 | 103 | 130 | 299 |
| Total | 892 | 665 | 431 | 1988 |
Physician-reported (non-FRS) vs. study-calculated FRS
Study-calculated FRS stratification| Low | Intermediate | High | Total | |
|---|---|---|---|---|
| Physician-reported risk stratification | ||||
| Low | 570 | 250 | 86 | 906 |
| Intermediate | 256 | 312 | 215 | 783 |
| High | 66 | 103 | 130 | 299 |
| Total | 892 | 665 | 431 | 1988 |
| Low | Intermediate | High | Total | |
|---|---|---|---|---|
| Physician-reported risk stratification | ||||
| Low | 570 | 250 | 86 | 906 |
| Intermediate | 256 | 312 | 215 | 783 |
| High | 66 | 103 | 130 | 299 |
| Total | 892 | 665 | 431 | 1988 |
Physician-reported (FRS) vs. study-calculated FRS
Study-calculated FRS stratification| Low | Intermediate | High | Total | |
|---|---|---|---|---|
| Physician-reported risk stratification | ||||
| Low | 377 | 196 | 52 | 625 |
| Intermediate | 43 | 140 | 127 | 310 |
| High | 2 | 20 | 69 | 91 |
| Total | 422 | 356 | 248 | 1026 |
| Low | Intermediate | High | Total | |
|---|---|---|---|---|
| Physician-reported risk stratification | ||||
| Low | 377 | 196 | 52 | 625 |
| Intermediate | 43 | 140 | 127 | 310 |
| High | 2 | 20 | 69 | 91 |
| Total | 422 | 356 | 248 | 1026 |
Physician-reported (FRS) vs. study-calculated FRS
Study-calculated FRS stratification| Low | Intermediate | High | Total | |
|---|---|---|---|---|
| Physician-reported risk stratification | ||||
| Low | 377 | 196 | 52 | 625 |
| Intermediate | 43 | 140 | 127 | 310 |
| High | 2 | 20 | 69 | 91 |
| Total | 422 | 356 | 248 | 1026 |
| Low | Intermediate | High | Total | |
|---|---|---|---|---|
| Physician-reported risk stratification | ||||
| Low | 377 | 196 | 52 | 625 |
| Intermediate | 43 | 140 | 127 | 310 |
| High | 2 | 20 | 69 | 91 |
| Total | 422 | 356 | 248 | 1026 |
Table 5 and Figure 2 illustrate the percentage of patients in each risk category who were recommended statin therapy at the second visit, based on their risk assessment. Although statin initiation was recommended for 92% of all patients who were classified by their treating physicians as high risk, this was true for only 56% of the truly high-risk patients (as classified by the study-calculated FRS).
Statin initiation according to gender and risk stratification
Patient risk category, according to the treating physician| Men, n = 1771 | 4.7% | 47% | 93% | <0.001 |
| Women, 1241 | 5.4% | 55% | 91% | <0.001 |
| All, n = 3012 | 5.0% | 50% | 92% | <0.001 |
| Patient risk category, based on the study-calculated FRS | ||||
| Men, n = 1770 | 16% | 32% | 54% | <0.001 |
| Women, n = 1241 | 20% | 41% | 68% | <0.001 |
| All, n = 3011 | 18% | 35% | 56% | <0.001 |
| Men, n = 1771 | 4.7% | 47% | 93% | <0.001 |
| Women, 1241 | 5.4% | 55% | 91% | <0.001 |
| All, n = 3012 | 5.0% | 50% | 92% | <0.001 |
| Patient risk category, based on the study-calculated FRS | ||||
| Men, n = 1770 | 16% | 32% | 54% | <0.001 |
| Women, n = 1241 | 20% | 41% | 68% | <0.001 |
| All, n = 3011 | 18% | 35% | 56% | <0.001 |
Statin initiation according to gender and risk stratification
Patient risk category, according to the treating physician| Men, n = 1771 | 4.7% | 47% | 93% | <0.001 |
| Women, 1241 | 5.4% | 55% | 91% | <0.001 |
| All, n = 3012 | 5.0% | 50% | 92% | <0.001 |
| Patient risk category, based on the study-calculated FRS | ||||
| Men, n = 1770 | 16% | 32% | 54% | <0.001 |
| Women, n = 1241 | 20% | 41% | 68% | <0.001 |
| All, n = 3011 | 18% | 35% | 56% | <0.001 |
| Men, n = 1771 | 4.7% | 47% | 93% | <0.001 |
| Women, 1241 | 5.4% | 55% | 91% | <0.001 |
| All, n = 3012 | 5.0% | 50% | 92% | <0.001 |
| Patient risk category, based on the study-calculated FRS | ||||
| Men, n = 1770 | 16% | 32% | 54% | <0.001 |
| Women, n = 1241 | 20% | 41% | 68% | <0.001 |
| All, n = 3011 | 18% | 35% | 56% | <0.001 |
Statin initiation stratified according to risk for all patients (n = 3015).
Statin initiation stratified according to risk for all patients (n = 3015).
Conclusion
This multicentre, prospective study examined ‘real-world’ primary care practice patterns for primary prevention of cardiovascular disease. Primary care physicians reported that they were most likely to use the FRS for cardiovascular risk stratification. However, regardless of the method of risk assessment used by physicians, there was only fair agreement with the study-calculated FRS, even when physicians reported using the FRS. Although the physician-estimated cardiovascular risk appeared to appropriately guide lipid management through statin therapy, the initial misclassification of risk corresponded to suboptimal statin recommendations for patients at high risk for cardiovascular disease.
Depending on the method utilized, the resultant risk stratification may vary, which may lead to significant differences in subsequent management choices and outcomes. A large prospective case–cohort study directly compared several risk methods (FRS, Adult Treatment Panel III [ATP-III], and RRS), which resulted in risk scores ranging from 6 to 41% for a 10-year risk of ≥10% cardiovascular risk in a given population.14 However, specific patient characteristics, ease of use, pattern of practice, or data availability may guide the treating physician's choice of method. A US study demonstrated that although 92% of physicians were aware of risk stratification tools, they were only used in 41% of patients, with only a fraction of the latter being used to guide subsequent treatment decisions.15 A recent cross-sectional study surveyed 846 primary care physicians across Canada, and 68.9% of physicians reported using the FRS as their primary method of cardiovascular risk assessment.16 As our study demonstrates, even when physicians reported using the FRS, there was only fair agreement between the treating physicians' risk assessment and the study-calculated FRS. Although this raises concern about the actual usage or the ability to accurately apply the reported risk stratification method; given the fair agreement across all methods, perhaps in practice, the actual choice of method for risk stratification may not be as important as the mere use of any objective risk assessment method. In previous ACS studies, several objective risk assessment methods were compared with the physicians' subjective global risk assessment. The former were demonstrated to be superior in providing an additional prognostic value, with potentially improved management and outcomes.17
In comparison with the study-calculated FRS, the overall results suggest that physicians underestimated a significant proportion of patients with high risk, with consequent implications for management decisions. As demonstrated in Figure 2, when patients were identified as high risk by the treating physician, statins were recommended for over 90% of these patients, which corresponds to the CCS dyslipidemia guidelines.6,7 However, also illustrated by Figure 2, when these patients were re-assessed by the study-calculated FRS, statin therapy was actually recommended to just over half of patients who truly had a high cardiovascular risk. This finding is supported by previous data in the Canadian primary care physician population, which found that almost a third of the surveyed physicians were also unaware of the defining point for high risk (>20% 10-year FRS cardiovascular risk).16 This misunderstanding may have contributed to the misclassification of risk and underestimation of the truly high-risk patients, with a consequent effect on the subsequent lipid management decisions. This care gap is not unique to Canada, as similar findings exist in other countries; for example, a European study demonstrated that statins were only prescribed in 47% of patients with hypercholesterolaemia.18
The main strength of the study includes the PARADIGM study design, as it is a nation-wide registry with a large sample size. However, PARADIGM was not a population-based sampling of prescribers and patients, as physicians were recruited from a subset population of those with high statin prescribing patterns. Despite this limitation, these results likely represent more conservative findings, and true practice may be even more discordant with guidelines, which provides reason and an even greater impetus for improvement. Other study limitations include a clustering of responses, and the unrecorded rationale behind the physician's choice of cardiovascular risk assessment or management. Other limitations that were beyond the scope of the study include the lack of long-term data and outcomes, information regarding medication adherence and patient education, and any decisions that were deferred or subsequently changed after the second visit.
A need clearly exists to improve real-world cardiovascular risk stratification in primary cardiovascular disease prevention. Our findings suggest the need for appropriate use of validated risk assessment methods for appropriate risk factor management for the primary prevention of cardiovascular disease. The true adherence to lipid guidelines was suboptimal, at least in part due to the physician's misclassification of the patients' cardiovascular risk, which may contribute to suboptimal risk factor management. Further studies regarding the rationales for choosing methods or subsequent management decisions may be useful to identify quality improvement strategies. Moreover, consideration may be given towards the more widespread application of any validated objective risk assessment method, given the persisting fair agreement between the treating physician's reported risk assessment and the study-calculated FRS (regardless of the method reportedly used for risk stratification, including the FRS as the method reportedly used). Finally, future studies may need to establish the optimal risk stratification method, with subsequent quality improvement strategies to appropriately apply validated risk scores in primary prevention.
Funding
This study was funded by CCRN through an unrestricted investigator initiated research grant from AstraZeneca Canada, Inc.
Conflict of interest: none declared.
Acknowledgement
This research was conducted with support from the Investigator-Sponsored Study Programme of AstraZeneca.
References
;Supplementary data
Abstract
To quantify the prevalence of coronary artery calcification (CAC) in relation to cardiovascular risk factors in marathon runners, and to study its role for myocardial damage and coronary events.
In 108 apparently healthy male marathon runners aged ≥50 years, with ≥5 marathon competitions during the previous three years, the running history, Framingham risk score (FRS), CAC, and presence of myocardial late gadolinium enhancement (LGE) were measured. Control groups were matched by age (8:1) and FRS (2:1) from the Heinz Nixdorf Recall Study. The FRS in marathon runners was lower than in age-matched controls (7 vs. 11%, P < 0.0001). However, the CAC distribution was similar in marathon runners and age-matched controls (median CAC: 36 vs. 38, P = 0.36) and higher in marathon runners than in FRS-matched controls (median CAC: 36 vs. 12, P = 0.02). CAC percentile values and number of marathons independently predicted the presence of LGE (prevalence = 12%) (P = 0.02 for both). During follow-up after 21.3 ± 2.8 months, four runners with CAC ≥ 100 experienced coronary events. Event-free survival was inversely related to CAC burden (P = 0.018).
Conventional cardiovascular risk stratification underestimates the CAC burden in presumably healthy marathon runners. As CAC burden and frequent marathon running seem to correlate with subclinical myocardial damage, an increased awareness of a potentially higher than anticipated coronary risk is warranted.
Introduction
Regular physical exercise improves the cardiovascular risk profile and reduces cardiovascular disease (CVD) morbidity and mortality.1,2 Vigorous exercise, on the other hand, increases the short-term risk of coronary events.3 Coronary atherosclerosis is the main underlying cause of exercise-related coronary events not only among elderly persons unaccustomed to exercise,4 but also in adult athletes including marathon runners.5,6
Over the past decades, the number of recreational marathon runners, including those at older age, is constantly rising. This trend may have implications for pre-participation cardiovascular risk stratification. Identification of marathon runners at risk is difficult and the need for cardiovascular medical examinations remains controversial.7,8 The risk of sudden cardiac death associated with marathon running has been suggested to be too low to recommend routine screening for coronary artery disease (CAD).9 In master athletes, pre-participation medical evaluations are nonetheless advised as a prudent measure before entering master sports training programmes.8,10 Standard clinical exercise tests can, however, be normal, even in the presence of rupture-prone coronary plaques.5,11,12
Based on prospective studies in various cohorts,13 it is speculated that advanced coronary artery calcification (CAC) in endurance athletes may be associated with an increased risk of cardiac events.5 Yet, the role of subclinical coronary atherosclerosis in cardiovascular risk assessment has not been studied in marathon runners. In patients with CAD, the presence of cardiac magnetic resonance imaging (cMRI)-based myocardial late gadolinium enhancement (LGE) may reflect prior myocardial damage and is associated with an impaired prognosis,14 but its association with subclinical CAC burden in healthy marathon runners is unknown.
This study was designed to quantify the prevalence of CAC in relation to cardiovascular risk factors in marathon runners, and to study its role for myocardial damage and coronary events.
Methods
Details on the Marathon study design have been reported previously.15 Participants were recruited in three ways: 1) an advertisement in a German marathon journal (‘Runners World’), 2) a press conference during inauguration of the study, and 3) inclusion of colleagues and friends of participants, if inclusion criteria were met. Matched control groups were selected from the Heinz Nixdorf Recall Study (HNRS).16 Both studies were approved by the local ethics committee and by the National Institute of Radiation Protection (Bundesamt für Strahlenschutz, Munich, Germany). All participants gave written informed consent prior to participation in both studies including informed consent for clinical follow-up and evaluation of hospital records.
Inclusion and exclusion criteria
Males ≥50 years were eligible, if they had completed at least five full-distance marathons (42.195 km) during the preceding three years. Exclusion criteria comprised history of established heart disease, diabetes mellitus, angina pectoris, and renal failure, musculo-skeletal disease at inclusion preventing future regular marathon running, psychiatric disease, and unwillingness to give informed consent.15 Two males were excluded from the study because of prior unreported myocardial infarction in one and severe renal failure because of untreated prostate disease in another.
Cardiovascular risk factors
Details on cardiovascular risk factor quantification and laboratory measurements have been described elsewhere.15,16 Blood pressure was measured with an automated oscillometric blood pressure device (Omron 705-CP, Omron, Germany). Current smoking was defined as a history of cigarette smoking during the past year. Participants were defined diabetic if they either reported a physician's diagnosis of diabetes, if they were taking anti-diabetic medication, or if their fasting glucose level was >126 mg/dL. All questionnaires, including those to quantify weekly exercise,17 interviews, and test protocols were identically used in both studies. The Framingham risk score (FRS) was computed as previously described.16
Electron-beam computed tomography
Non-enhanced electron-beam computed tomography (EBCT) scans were performed on C-150 scanners (GE Imatron, South San Francisco, USA). EBCT scans for the studies were obtained at three sites with identical scanning protocols as previously described.18 The Agatston CAC score was quantified and percentile CAC values were calculated based on data from the HNRS.18 The CAC score was not given to participants or to general practitioners in both studies.
Cardiac magnetic resonance imaging
cMRI scans were performed in the marathon study but not in the HNRS. All examinations were performed on a 1.5 T MR scanner equipped with high-performance gradients (Magnetom Avanto, Siemens, Erlangen, Germany). An inversion recovery fast low angle shot sequence (IR-turboFLASH: TR 8.0 ms, TE 4.0 ms, TI 180–240 ms, FA 20°) was acquired in short- and long-axis views 10–15 min after injection of 0.2 mmol/kg body weight of gadolinium-diethylene triamine pentaacetic acid (DTPA) (Magnevist, Schering AG, Berlin, Germany) to identify LGE. Pattern and extent of LGE were assessed using short- and long-axis views19 and were defined as present only if detectable in two orthogonal planes. A repeat cMRI study was performed when LGE was detected.
Follow-up and definition of coronary events
Follow-up information was obtained from annual questionnaires and personal communication. Events were confirmed from hospital records. Coronary events were defined as sudden coronary death, myocardial infarction, and coronary revascularization.
Statistical analysis
For comparison with the general population, two groups matching the marathon runners (group I) were drawn from the HNRS cohort, restricted to males without CAD, aged ≥50 (n = 1842). These were group II: 1:8 matching in four-year age classes, group III: 1:2 matching within ±3 years of age, within ±3 kg/m2 body mass index (BMI), within ±4% Framingham risk per 10 years, and by smoking status (present/former/never smokers). Furthermore, the matched cohort group III was restricted to HNRS participants without a history of stroke or diabetes (n = 1597). Matching was performed using PROC SURVEYSELECT of SAS (SAS Institute Inc., Cary, NC, USA) to generate group II and the algorithm described in Schröder et al.20 to generate group III.
Data were presented as mean ± SD, median—25th and 75th percentiles (Q1 and Q3), or proportions, where appropriate. Correlations involving CAC score were calculated according to Spearman, associations with physical activity parameters were also analysed with linear regression analyses for log-transformed (CAC + 1). To compare matching factors between groups, the Mann–Whitney U test, χ2 test, or Fisher's exact test were employed. To evaluate group effects controlling for matching factors, general linear or logistic models (PROC GLM or PROC LOGISTIC of SAS) were used. Because of the strongly skew CAC distribution, models for CAC were based on ranks. Predictive models for CAC were also calculated using general linear models, with the Agatston score transformed as log2(CAC + 1). All linear regression models were inspected by analysis of residuals and checked for nonlinear dependencies. Except models for log2(CAC + 1) there were no abnormalities.
Presence of LGE was modelled by logistic regression in one and two variables. Because of the low number of LGE, P-values from a two-variable model, comprising number of marathons (logarithmized), and CAC percentile values, were recalculated with exact logistic regression using LogXact (Cytel Software Corporation, Cambridge, MA, USA).
Event-free survival rates were estimated following the Kaplan–Meier method and overall group differences were evaluated by log-rank statistics. In addition, a Cox regression model with log-transformed CAC—log2(CAC + 1)—as independent variable was calculated.
Results
One hundred and eight male runners aged 50–72 years were included in the study. They had completed 20 marathons (median value, Q1–Q3: 14–42), had started marathon running nine years ago (Q1–Q3: 7–16), and trained 55 km (approximately 35 miles) (Q1–Q3: 45–65) on five days per week throughout the year.
Matching
Our attempt to match two males out of 1597 eligible males from the HNRS with each marathon runner by age, BMI, and FRS did not result in an equal FRS but in a lower FRS in marathon runners than in group-III controls (7.0 ± 3.6 vs. 7.7 ± 3.4%, P = 0.03) (Table 1).
Demographic variables and risk factors
Participants of the Heinz Nixdorf Recall Study| P-value group I vs. group II | P-value group I vs. group III | ||||
|---|---|---|---|---|---|
| Marathon runners (group I) | Age-matched controls (8:1) (group II) | Controls matched for age and risk factors (2:1) (group III) | |||
| n | 108 | 864 | 216 | n.a. | n.a. |
| Age (years) | 57.2 ± 5.7 | 57.2 ± 5.9 | 57.1 ± 5.6 | 0.96 | 0.93 |
| BMI | 24.0 ± 2.3 | 28.1 ± 4.0 | 24.9 ± 2.1 | <0.0001 | 0.0004 |
| Systolic blood pressure (mmHg) | 121 ± 14 | 137 ± 18 | 127 ± 14 | <0.0001 | 0.02 |
| History of hypertension (%) | 12.0 | 40.8 | 28.4 | <0.0001 | 0.005 |
| Total cholesterol (mg/dL) | 227 ± 42 | 228 ± 38 | 215 ± 32 | 0.91 | 0.0004 |
| LDL cholesterol (mg/dL) | 121 ± 29 | 147 ± 36 | 131 ± 31 | <0.0001 | 0.05 |
| HDL cholesterol (mg/dL) | 73.8 ± 17.3 | 51.9 ± 14.7 | 60.6 ± 14.7 | <0.0001 | <0.0001 |
| Smoking status | |||||
| Current (%) | 4.6 | 28.4 | 4.6 | <0.0001 | n.a. |
| Former (%) | 51.9 | 42.1 | 51.9 | 0.41 | n.a. |
| Diabetes (%) | 0 | 8.6 | 0 | 0.002 | n.a. |
| 10-year Framingham risk score | 7 (4–9) | 11 (9–18) | 7 (6–9) | <0.0001 | 0.03 |
| History of stroke (%) | 0 | 2.2 | 0 | 0.12 | n.a. |
| Weekly exercise (MET/week) | 4686 ± 2285 | 1389 ± 1876 | 1748 ± 2200 | <0.0001 | <0.0001 |
| Resting heart rate (b.p.m.) | 65 ± 10 | 76 ± 12 | 74 ± 11 | <0.0001 | <0.0001 |
| P-value group I vs. group II | P-value group I vs. group III | ||||
|---|---|---|---|---|---|
| Marathon runners (group I) | Age-matched controls (8:1) (group II) | Controls matched for age and risk factors (2:1) (group III) | |||
| n | 108 | 864 | 216 | n.a. | n.a. |
| Age (years) | 57.2 ± 5.7 | 57.2 ± 5.9 | 57.1 ± 5.6 | 0.96 | 0.93 |
| BMI | 24.0 ± 2.3 | 28.1 ± 4.0 | 24.9 ± 2.1 | <0.0001 | 0.0004 |
| Systolic blood pressure (mmHg) | 121 ± 14 | 137 ± 18 | 127 ± 14 | <0.0001 | 0.02 |
| History of hypertension (%) | 12.0 | 40.8 | 28.4 | <0.0001 | 0.005 |
| Total cholesterol (mg/dL) | 227 ± 42 | 228 ± 38 | 215 ± 32 | 0.91 | 0.0004 |
| LDL cholesterol (mg/dL) | 121 ± 29 | 147 ± 36 | 131 ± 31 | <0.0001 | 0.05 |
| HDL cholesterol (mg/dL) | 73.8 ± 17.3 | 51.9 ± 14.7 | 60.6 ± 14.7 | <0.0001 | <0.0001 |
| Smoking status | |||||
| Current (%) | 4.6 | 28.4 | 4.6 | <0.0001 | n.a. |
| Former (%) | 51.9 | 42.1 | 51.9 | 0.41 | n.a. |
| Diabetes (%) | 0 | 8.6 | 0 | 0.002 | n.a. |
| 10-year Framingham risk score | 7 (4–9) | 11 (9–18) | 7 (6–9) | <0.0001 | 0.03 |
| History of stroke (%) | 0 | 2.2 | 0 | 0.12 | n.a. |
| Weekly exercise (MET/week) | 4686 ± 2285 | 1389 ± 1876 | 1748 ± 2200 | <0.0001 | <0.0001 |
| Resting heart rate (b.p.m.) | 65 ± 10 | 76 ± 12 | 74 ± 11 | <0.0001 | <0.0001 |
LDL, low-density lipoprotein; HDL, high-density lipoprotein; BMI, body mass index; b.p.m., beats per minute; MET, metabolic equivalent; n.a., not available. All subjects were free of overt coronary artery disease, i.e. history of myocardial infarction or coronary revascularization. Data are presented as mean ± SD, proportions (%), or median values. The numbers in brackets indicate Q1–Q3, i.e. 25th and 75th percentile. All group I/group II comparisons adjusted for age, all group I/group III comparisons (excepting matching factors) adjusted for age, BMI, Framingham risk, smoking status.
Demographic variables and risk factors
Participants of the Heinz Nixdorf Recall Study| P-value group I vs. group II | P-value group I vs. group III | ||||
|---|---|---|---|---|---|
| Marathon runners (group I) | Age-matched controls (8:1) (group II) | Controls matched for age and risk factors (2:1) (group III) | |||
| n | 108 | 864 | 216 | n.a. | n.a. |
| Age (years) | 57.2 ± 5.7 | 57.2 ± 5.9 | 57.1 ± 5.6 | 0.96 | 0.93 |
| BMI | 24.0 ± 2.3 | 28.1 ± 4.0 | 24.9 ± 2.1 | <0.0001 | 0.0004 |
| Systolic blood pressure (mmHg) | 121 ± 14 | 137 ± 18 | 127 ± 14 | <0.0001 | 0.02 |
| History of hypertension (%) | 12.0 | 40.8 | 28.4 | <0.0001 | 0.005 |
| Total cholesterol (mg/dL) | 227 ± 42 | 228 ± 38 | 215 ± 32 | 0.91 | 0.0004 |
| LDL cholesterol (mg/dL) | 121 ± 29 | 147 ± 36 | 131 ± 31 | <0.0001 | 0.05 |
| HDL cholesterol (mg/dL) | 73.8 ± 17.3 | 51.9 ± 14.7 | 60.6 ± 14.7 | <0.0001 | <0.0001 |
| Smoking status | |||||
| Current (%) | 4.6 | 28.4 | 4.6 | <0.0001 | n.a. |
| Former (%) | 51.9 | 42.1 | 51.9 | 0.41 | n.a. |
| Diabetes (%) | 0 | 8.6 | 0 | 0.002 | n.a. |
| 10-year Framingham risk score | 7 (4–9) | 11 (9–18) | 7 (6–9) | <0.0001 | 0.03 |
| History of stroke (%) | 0 | 2.2 | 0 | 0.12 | n.a. |
| Weekly exercise (MET/week) | 4686 ± 2285 | 1389 ± 1876 | 1748 ± 2200 | <0.0001 | <0.0001 |
| Resting heart rate (b.p.m.) | 65 ± 10 | 76 ± 12 | 74 ± 11 | <0.0001 | <0.0001 |
| P-value group I vs. group II | P-value group I vs. group III | ||||
|---|---|---|---|---|---|
| Marathon runners (group I) | Age-matched controls (8:1) (group II) | Controls matched for age and risk factors (2:1) (group III) | |||
| n | 108 | 864 | 216 | n.a. | n.a. |
| Age (years) | 57.2 ± 5.7 | 57.2 ± 5.9 | 57.1 ± 5.6 | 0.96 | 0.93 |
| BMI | 24.0 ± 2.3 | 28.1 ± 4.0 | 24.9 ± 2.1 | <0.0001 | 0.0004 |
| Systolic blood pressure (mmHg) | 121 ± 14 | 137 ± 18 | 127 ± 14 | <0.0001 | 0.02 |
| History of hypertension (%) | 12.0 | 40.8 | 28.4 | <0.0001 | 0.005 |
| Total cholesterol (mg/dL) | 227 ± 42 | 228 ± 38 | 215 ± 32 | 0.91 | 0.0004 |
| LDL cholesterol (mg/dL) | 121 ± 29 | 147 ± 36 | 131 ± 31 | <0.0001 | 0.05 |
| HDL cholesterol (mg/dL) | 73.8 ± 17.3 | 51.9 ± 14.7 | 60.6 ± 14.7 | <0.0001 | <0.0001 |
| Smoking status | |||||
| Current (%) | 4.6 | 28.4 | 4.6 | <0.0001 | n.a. |
| Former (%) | 51.9 | 42.1 | 51.9 | 0.41 | n.a. |
| Diabetes (%) | 0 | 8.6 | 0 | 0.002 | n.a. |
| 10-year Framingham risk score | 7 (4–9) | 11 (9–18) | 7 (6–9) | <0.0001 | 0.03 |
| History of stroke (%) | 0 | 2.2 | 0 | 0.12 | n.a. |
| Weekly exercise (MET/week) | 4686 ± 2285 | 1389 ± 1876 | 1748 ± 2200 | <0.0001 | <0.0001 |
| Resting heart rate (b.p.m.) | 65 ± 10 | 76 ± 12 | 74 ± 11 | <0.0001 | <0.0001 |
LDL, low-density lipoprotein; HDL, high-density lipoprotein; BMI, body mass index; b.p.m., beats per minute; MET, metabolic equivalent; n.a., not available. All subjects were free of overt coronary artery disease, i.e. history of myocardial infarction or coronary revascularization. Data are presented as mean ± SD, proportions (%), or median values. The numbers in brackets indicate Q1–Q3, i.e. 25th and 75th percentile. All group I/group II comparisons adjusted for age, all group I/group III comparisons (excepting matching factors) adjusted for age, BMI, Framingham risk, smoking status.
Risk factor distribution
Compared with age-matched controls, marathon runners had a 42% higher high-density lipoprotein cholesterol, an 18% lower low-density lipoprotein-cholesterol, a 19% lower rate of ever smoking, a 12% lower systolic blood pressure, and a 15% lower BMI (Table 1), resulting in a 51% lower mean 10 year FRS (7.0 ± 3.6 vs. 14.3 ± 8.2%, P < 0.0001).
Physical activity
Marathon runners had higher weekly metabolic equivalents (METs) and lower heart rates than both control groups (Table 1). We found no age-adjusted Spearman correlation between weekly METs and CAC in marathon runners (R2 = 0.02, P = 0.13) or in age-matched controls (R2 = 0.001, P = 0.36). In marathon runners, CAC was also not associated with years of running (R2 = 0.024, P = 0.12), with the number of marathon races completed (R2 = 0.007, P = 0.39), or with training mileage (R2 = 0.014, P = 0.23). Regression analyses revealed no hints for curve-linearity in any of these relations, and the respective 95% confidence intervals (CIs) of estimated slopes all included zero.
Prevalence and extent of coronary artery calcification
A zero CAC score was more frequent in marathon runners than in age-matched controls, but was similar when compared with FRS-matched controls (Table 2). The overall CAC score distribution was similar in marathon runners and age-matched controls (Table 2) with similar rates of CAC ≥ 100 in these groups (36.1 vs. 36.3%, P = 0.96) but higher rates in marathon runners when compared with FRS-matched controls (36.1 vs. 21.8%, P = 0.01) (Table 2).
Distribution of coronary artery calcification (CAC) measures in the three groups
Participants of the Heinz Nixdorf Recall Study| P-value group I vs. group II | P-value group I vs. group III | ||||
|---|---|---|---|---|---|
| Marathon runners (group I) | Age-matched controls (8:1) (group II) | Controls matched for age and risk factors (2:1) (group III) | |||
| log2(CAC + 1) (mean ± SD) | 4.1 ± 3.6 | 4.9 ± 3.3 | 3.8 ± 3.4 | 0.28 | 0.02 |
| CAC (Q1/median/Q3) | 0/36/217 | 3/38/187 | 0/12/78 | 0.36 | 0.02 |
| zero CAC (%) | 28.7 | 18.4 | 31.5 | 0.01 | 0.50 |
| CAC >75th percentile (%) | 25.0 | 24.2 | 14.8 | 0.85 | 0.01 |
| CAC 0 to <10 | 40.74 | 34.61 | 48.61 | ||
| CAC 10 to <100 | 23.15 | 29.05 | 29.63 | ||
| CAC 100 to <400 | 23.15 | 22.80 | 13.43 | 0.52 | 0.02 |
| CAC ≥400 | 12.96 | 13.54 | 8.33 |
| P-value group I vs. group II | P-value group I vs. group III | ||||
|---|---|---|---|---|---|
| Marathon runners (group I) | Age-matched controls (8:1) (group II) | Controls matched for age and risk factors (2:1) (group III) | |||
| log2(CAC + 1) (mean ± SD) | 4.1 ± 3.6 | 4.9 ± 3.3 | 3.8 ± 3.4 | 0.28 | 0.02 |
| CAC (Q1/median/Q3) | 0/36/217 | 3/38/187 | 0/12/78 | 0.36 | 0.02 |
| zero CAC (%) | 28.7 | 18.4 | 31.5 | 0.01 | 0.50 |
| CAC >75th percentile (%) | 25.0 | 24.2 | 14.8 | 0.85 | 0.01 |
| CAC 0 to <10 | 40.74 | 34.61 | 48.61 | ||
| CAC 10 to <100 | 23.15 | 29.05 | 29.63 | ||
| CAC 100 to <400 | 23.15 | 22.80 | 13.43 | 0.52 | 0.02 |
| CAC ≥400 | 12.96 | 13.54 | 8.33 |
Comparisons in continuous or binary measures adjusted for matching factors (age for group I/group II, age, body mass index, Framingham risk, smoking status for group I/group III).
Distribution of coronary artery calcification (CAC) measures in the three groups
Participants of the Heinz Nixdorf Recall Study| P-value group I vs. group II | P-value group I vs. group III | ||||
|---|---|---|---|---|---|
| Marathon runners (group I) | Age-matched controls (8:1) (group II) | Controls matched for age and risk factors (2:1) (group III) | |||
| log2(CAC + 1) (mean ± SD) | 4.1 ± 3.6 | 4.9 ± 3.3 | 3.8 ± 3.4 | 0.28 | 0.02 |
| CAC (Q1/median/Q3) | 0/36/217 | 3/38/187 | 0/12/78 | 0.36 | 0.02 |
| zero CAC (%) | 28.7 | 18.4 | 31.5 | 0.01 | 0.50 |
| CAC >75th percentile (%) | 25.0 | 24.2 | 14.8 | 0.85 | 0.01 |
| CAC 0 to <10 | 40.74 | 34.61 | 48.61 | ||
| CAC 10 to <100 | 23.15 | 29.05 | 29.63 | ||
| CAC 100 to <400 | 23.15 | 22.80 | 13.43 | 0.52 | 0.02 |
| CAC ≥400 | 12.96 | 13.54 | 8.33 |
| P-value group I vs. group II | P-value group I vs. group III | ||||
|---|---|---|---|---|---|
| Marathon runners (group I) | Age-matched controls (8:1) (group II) | Controls matched for age and risk factors (2:1) (group III) | |||
| log2(CAC + 1) (mean ± SD) | 4.1 ± 3.6 | 4.9 ± 3.3 | 3.8 ± 3.4 | 0.28 | 0.02 |
| CAC (Q1/median/Q3) | 0/36/217 | 3/38/187 | 0/12/78 | 0.36 | 0.02 |
| zero CAC (%) | 28.7 | 18.4 | 31.5 | 0.01 | 0.50 |
| CAC >75th percentile (%) | 25.0 | 24.2 | 14.8 | 0.85 | 0.01 |
| CAC 0 to <10 | 40.74 | 34.61 | 48.61 | ||
| CAC 10 to <100 | 23.15 | 29.05 | 29.63 | ||
| CAC 100 to <400 | 23.15 | 22.80 | 13.43 | 0.52 | 0.02 |
| CAC ≥400 | 12.96 | 13.54 | 8.33 |
Comparisons in continuous or binary measures adjusted for matching factors (age for group I/group II, age, body mass index, Framingham risk, smoking status for group I/group III).
Prevalence and predictors of myocardial late gadolinium enhancement
cMRI studies were performed in 102 subjects. Reasons for non-participation were a cochlear metal implant (n = 1), metal splinter in a rib (n = 1), claustrophobia (n = 1), refusal of contrast administration (n = 2), and poor image quality (n = 1). LGE was observed in 12 persons (12%) with n = 5 (42%) showing a subendocardial scar pattern typical of ischaemia and n = 7 (58%) with a mid-myocardial patchy pattern suggesting non-ischaemic origin. Runners with LGE had a higher CAC score vs. those without LGE [median CAC (Q1–Q3): 192 (129–603) vs. 26 (0–159), P = 0.0046]. In univariate analysis, the CAC score, CAC percentile values, and the number of marathons but not the FRS were associated with LGE (Table 3). In multivariable analysis, CAC percentile distribution and the number of marathons remained independently associated with the presence of LGE (Table 3). These associations were confirmed by exact logistic regression.
Univariate and multivariate analysis for predictors of myocardial late gadolinium enhancement (LGE)
Follow-up and eventsNo marathon runner died during 21.0 months [interquartile range (IQR) 18.6–24.0 months) of follow-up. Coronary events occurred in four runners (Table 4). Two of these were sudden (hard) coronary events and two others were revascularizations. The first runner with an event (CAC = 874, Table 4) was successfully resuscitated after 7 km during a 10 km race. Coronary angiography revealed significant stenoses (>80% lumen reduction) in all three vessels. The second runner with an event (CAC = 472, Table 4) underwent uneventful coronary artery bypass graft (CABG) surgery because of left main disease and significant angiographic two-vessel disease, which was identified during additional testing, as previously published in detail.11 Revascularization in the third event (CAC = 171, Table 4) was triggered by an electrocardiogram (EKG) performed after a marathon competition demonstrating ST-elevation. A subsequent echocardiogram showed septal wall motion abnormality, which was followed by invasive angiography, demonstrating significant left anterior descending stenosis and myocardial bridging of a septal branch. The fourth event (CAC = 128, Table 4) occurred just after moderate physical exercise. The participant was successfully resuscitated. Coronary angiography demonstrated significant three-vessel disease followed by CABG surgery. At present, all these runners are fit and well.
Risk factors and test results of participants with events during follow-up
| Normal rangea | |||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||
| Age (years) | 66 | 64 | 55 | 62 | |
| BMI (kg/m2) | 22.5 | 24.6 | 22.0 | 22.0 | <25 |
| Systolic blood pressure (mmHg) | 110/61 | 105/67b | 153/96 | 138/82 | <120/80 |
| History of hypertension | No | Yes | No | Yes | No |
| Total cholesterol (mg/dL) | 344 | 201 | 233 | 240 | <240 |
| LDL cholesterol (mg/dL) | 170 | 116 | 98 | 131 | <160 |
| HDL cholesterol (mg/dL) | 109 | 60 | 100 | 65 | >40 |
| Smoking status | Former | Never | Former | Former | Never |
| 10-year Framingham risk score (%) | 8 | 7 | 6 | 10 | The lower the better |
| CAC score (Agatston units) | 874 | 472 | 171 | 128 | zero CAC |
| CAC percentile rank | 86 | 81 | 73 | 60 | zero CAC |
| Myocardial LGE | Yes | No | Yes | Yes | No |
| Resting heart rate (b.p.m.) | 48 | 58 | 63 | 42 | 50–100 |
| Weekly MET | 4241 | 4806 | 8296 | 5054 | |
| Marathons completed (no.) | 14 | 22 | 65 | 140 | |
| Findings on invasive angiography | Three-VD | Two-VD | Myocardial bridge/One-VD | Three-VD | |
| Type of event | VT during exercise, stent | Stent/CABG | Stent | VT during exercise, CABG |
| Normal rangea | |||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||
| Age (years) | 66 | 64 | 55 | 62 | |
| BMI (kg/m2) | 22.5 | 24.6 | 22.0 | 22.0 | <25 |
| Systolic blood pressure (mmHg) | 110/61 | 105/67b | 153/96 | 138/82 | <120/80 |
| History of hypertension | No | Yes | No | Yes | No |
| Total cholesterol (mg/dL) | 344 | 201 | 233 | 240 | <240 |
| LDL cholesterol (mg/dL) | 170 | 116 | 98 | 131 | <160 |
| HDL cholesterol (mg/dL) | 109 | 60 | 100 | 65 | >40 |
| Smoking status | Former | Never | Former | Former | Never |
| 10-year Framingham risk score (%) | 8 | 7 | 6 | 10 | The lower the better |
| CAC score (Agatston units) | 874 | 472 | 171 | 128 | zero CAC |
| CAC percentile rank | 86 | 81 | 73 | 60 | zero CAC |
| Myocardial LGE | Yes | No | Yes | Yes | No |
| Resting heart rate (b.p.m.) | 48 | 58 | 63 | 42 | 50–100 |
| Weekly MET | 4241 | 4806 | 8296 | 5054 | |
| Marathons completed (no.) | 14 | 22 | 65 | 140 | |
| Findings on invasive angiography | Three-VD | Two-VD | Myocardial bridge/One-VD | Three-VD | |
| Type of event | VT during exercise, stent | Stent/CABG | Stent | VT during exercise, CABG |
Note that details on subject 2 have previously been reported.11
LGE, late gadolinium enhancement; VD, vessel disease; b.p.m., beats per minute; VT, ventricular tachycardia; CABG, coronary artery bypass graft; HDL, high-density lipoprotein; LDL, low-density lipoprotein; CAC, coronary artery calcium; MET, metabolic equivalent; no., number.
bOn 5 mg Ramipril (Sanofi Aventis, Frankfurt, Germany) once daily.
Risk factors and test results of participants with events during follow-up
Subjects with an event during follow-up| Normal rangea | |||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||
| Age (years) | 66 | 64 | 55 | 62 | |
| BMI (kg/m2) | 22.5 | 24.6 | 22.0 | 22.0 | <25 |
| Systolic blood pressure (mmHg) | 110/61 | 105/67b | 153/96 | 138/82 | <120/80 |
| History of hypertension | No | Yes | No | Yes | No |
| Total cholesterol (mg/dL) | 344 | 201 | 233 | 240 | <240 |
| LDL cholesterol (mg/dL) | 170 | 116 | 98 | 131 | <160 |
| HDL cholesterol (mg/dL) | 109 | 60 | 100 | 65 | >40 |
| Smoking status | Former | Never | Former | Former | Never |
| 10-year Framingham risk score (%) | 8 | 7 | 6 | 10 | The lower the better |
| CAC score (Agatston units) | 874 | 472 | 171 | 128 | zero CAC |
| CAC percentile rank | 86 | 81 | 73 | 60 | zero CAC |
| Myocardial LGE | Yes | No | Yes | Yes | No |
| Resting heart rate (b.p.m.) | 48 | 58 | 63 | 42 | 50–100 |
| Weekly MET | 4241 | 4806 | 8296 | 5054 | |
| Marathons completed (no.) | 14 | 22 | 65 | 140 | |
| Findings on invasive angiography | Three-VD | Two-VD | Myocardial bridge/One-VD | Three-VD | |
| Type of event | VT during exercise, stent | Stent/CABG | Stent | VT during exercise, CABG |
| Normal rangea | |||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||
| Age (years) | 66 | 64 | 55 | 62 | |
| BMI (kg/m2) | 22.5 | 24.6 | 22.0 | 22.0 | <25 |
| Systolic blood pressure (mmHg) | 110/61 | 105/67b | 153/96 | 138/82 | <120/80 |
| History of hypertension | No | Yes | No | Yes | No |
| Total cholesterol (mg/dL) | 344 | 201 | 233 | 240 | <240 |
| LDL cholesterol (mg/dL) | 170 | 116 | 98 | 131 | <160 |
| HDL cholesterol (mg/dL) | 109 | 60 | 100 | 65 | >40 |
| Smoking status | Former | Never | Former | Former | Never |
| 10-year Framingham risk score (%) | 8 | 7 | 6 | 10 | The lower the better |
| CAC score (Agatston units) | 874 | 472 | 171 | 128 | zero CAC |
| CAC percentile rank | 86 | 81 | 73 | 60 | zero CAC |
| Myocardial LGE | Yes | No | Yes | Yes | No |
| Resting heart rate (b.p.m.) | 48 | 58 | 63 | 42 | 50–100 |
| Weekly MET | 4241 | 4806 | 8296 | 5054 | |
| Marathons completed (no.) | 14 | 22 | 65 | 140 | |
| Findings on invasive angiography | Three-VD | Two-VD | Myocardial bridge/One-VD | Three-VD | |
| Type of event | VT during exercise, stent | Stent/CABG | Stent | VT during exercise, CABG |
Note that details on subject 2 have previously been reported.11
LGE, late gadolinium enhancement; VD, vessel disease; b.p.m., beats per minute; VT, ventricular tachycardia; CABG, coronary artery bypass graft; HDL, high-density lipoprotein; LDL, low-density lipoprotein; CAC, coronary artery calcium; MET, metabolic equivalent; no., number.
bOn 5 mg Ramipril (Sanofi Aventis, Frankfurt, Germany) once daily.
Distribution of CAC in runners with events was as follows—CAC <100: 0 of 69 (0%); CAC 100 to <400: two of 25 (8%), and CAC ≥400: two of 14 (14.3%). The difference in event rates among CAC groups reached statistical significance using log-rank analysis but just failed to reach statistical significance using Cox regression analysis (Figure 1).
Kaplan–Meier estimates of event-free survival by extent of coronary artery calcification (CAC). No marathon runners with CAC <100 experienced a coronary event, while 8% and 14.3% of those with CAC 100 to <400 and ≥400, respectively, required revascularization during follow-up. Using Cox regression analysis, hazard ratios for a two-fold increase in log2(CAC+1) were: hazard ratio = 1.51, 95% confidence interval = 0.97–2.36, P = 0.07. The numbers pertain to the subjects with events in Table 3.
Kaplan–Meier estimates of event-free survival by extent of coronary artery calcification (CAC). No marathon runners with CAC <100 experienced a coronary event, while 8% and 14.3% of those with CAC 100 to <400 and ≥400, respectively, required revascularization during follow-up. Using Cox regression analysis, hazard ratios for a two-fold increase in log2(CAC+1) were: hazard ratio = 1.51, 95% confidence interval = 0.97–2.36, P = 0.07. The numbers pertain to the subjects with events in Table 3.
Discussion
The present study was designed to examine the prevalence of subclinical atherosclerosis in relation to cardiovascular risk factors and their role for myocardial damage and outcome in accomplished recreational marathon runners. To our surprise, given the substantial evidence that physical activity reduces CAD event rates,1,2,21 a CAC score ≥100 was present in 36% of runners, which was not different from age-matched controls, even though the FRS was much lower. Further, the CAC score exceeded that in controls matched for age and FRS. The CAC score was predictive of myocardial damage, which was evidenced by LGE in 12% of runners. Our outcome data suggest that higher CAC scores may be associated with higher rates of events. There are several possible explanations for these findings.
With respect to the mismatch between FRS and the extent of CAC in marathon runners, many of the runners have commenced marathon running in middle-age. Consequently, their cardiovascular risk factors could have been reduced by exercise training and may not reflect their life-long risk exposure. In fact, more than half of our runners were previous smokers and 5% of runners reported active smoking. This would also explain the comparatively low CAC scores in controls matched for age and FRS, which may have had life-long protection from the atherogenic effect of cardiovascular risk factor exposure. The clinical implication of this possibility is that standard risk factor estimates may lead runners and their physicians to underestimate the athletes' true risk. Risk stratification in marathon runners is further rendered difficult by improved microvascular function in marathon runners, which can compensate for severe epicardial plaque burden and thereby concealing the true extent of coronary atherosclerosis.11 This may in part explain why all runners in our study were asymptomatic at rest and during running despite considerable atherosclerosis in so many.
In our study, CAC scores were not related to any measure of physical activity in any of the groups. Given the expected population-wide annual increase in CAC of 15–20%,18 regular marathon running seems not to protect runners from CAC progression once CAC is present. In fact, we even cannot exclude the possibility that exercise to this degree has deleterious effects on coronary arteries. This seems unlikely given the substantial experimental22 and clinical1,2,23,24 evidence for the benefits of regular physical activity, but no epidemiological studies have so far examined individuals engaged in such prodigious amounts of exercise as our marathon runners. Several mechanisms may be involved: regular exhaustive exercise during marathon and its required training may induce a rise in vascular oxidative stress because of a high-flow, high-pressure condition, to a point at which it challenges anti-oxidative capacity.22 Bursts of inflammatory cytokines, which almost invariably occur during marathon running,25 may also accelerate the atherosclerotic disease process and impair intramyocardial microvascular integrity, whereas no ischaemia is detected during a short-term diagnostic exercise protocol.
The possibility that marathon running and the required training aggravates pre-existing non-calcified atherosclerosis and has a role in LGE development is clearly speculative based on our cross-sectional data. However, it is interesting given recent reports of myocardial injury during marathon running and the observation of prevalent myocardial damage in our runners. Others have demonstrated increases in myocardial troponin levels in recreational marathon runners and other endurance athletes.26–29 The cause of such possible myocardial damage is unclear, but unlikely owing to epicardial coronary artery obstruction. Evidence of myocardial damage was found in 12% of our 108 runners. A pattern highly suggestive of myocardial ischaemia was seen in 42% of these, whereas the others demonstrated more patchy defects. We have previously shown that infusion of small particles of 10–100 µm in diameter into porcine coronary arteries leads to haemorrhagic and patchy patterns of myocardial damage, depending on particle size.30 Embolization of microthrombi or atherosclerotic plaque material into the microvasculature is also conceivable during marathon running, because excessive mechanical forces may put strain on plaques and thereby cause plaque erosion or fissuring with subsequent epicardial thrombus formation8 and microembolization.31 An increased exercise-induced thrombogenicity from increased catecholamine-induced platelet aggregation, or an imbalance in fibrinolytic/prothrombotic factors32,33 may also have a role in such thrombus formation. It is therefore possible that both the myocardial injury reported after marathon running26–29 and the myocardial damage in our marathon runners are in part due to small thrombotic or even atherosclerotic emboli.
The presence of myocardial LGE has recently been shown to predict cardiac events in patients with CAD.14 In marathon runners, such damaged myocardium may be a substrate for an increased susceptibility to arrhythmias in response to increased exercise-related catecholamine levels,8 and hence may contribute to cardiac events. In our study, CAC scores were higher in those runners with LGE, supporting a pathophysiological link between epicardial subclinical plaque burden and intramyocardial microvascular damage, as indicated above. Even though CAC is not a measure of plaque vulnerability at that site,34 the increasing rate of coronary events in parallel with increasing CAC scores may indicate increased plaque vulnerability or susceptibility for plaque rupture or fissuring somewhere else in the coronary tree. The precise mechanism by which elevated epicardial plaque burden may increase the likelihood of myocardial damage and vulnerability, remains to be shown.
Limitations
Our data do not apply to women and may not be representative for all marathon runners, as we cannot exclude recruitment bias. Participants may have had previous risk factors, a recent reduction in exercise capacity or recently discovered CVD in a relative. However, we have excluded all subjects with known CVD, diabetes, or any symptoms of CVD, and participants have been running regularly for nine years. The risk factor profile in our cohort is therefore typical for many marathon runners and is expected to be worse in many others. This pertains in particular to diabetic athletes, who have been excluded from this study.
Because of different recruitment strategies and inclusion criteria between the two studies, our findings are subject to selection bias: marathon runners were self-referred because they could not be randomly selected as the participants in the HNRS. They also had to be fit and healthy beyond age 50 to be included, while this was not the case in the HNRS.
Our cohort of marathon runners is heterogeneous with regard to duration of regular physical exercise and marathon running, as evidenced by the interquartile ranges of years of active running, number of marathons completed, and the weekly training mileage. Participants may also differ in their engagement in sports other than marathon running. We believe, though, that our findings reflect the typical spectrum of risk factor and atherosclerosis burden in males >50 years participating in marathons.
It is conceivable that the ratio of calcified and non-calcified atherosclerotic plaque differs among persons who are regularly exposed to exhaustive exercise and those who are not, because repetitive increases in shear stress and mechanical forces may predominantly impact on the calcified plaque component. Currently, there are no data to support this hypothesis, which can only be assessed non-invasively by additional administration of contrast agent and high-resolution computed tomographic techniques.
We have discussed oxidative stress, microembolization, bursts of inflammation or increased thrombogenicity as potential mechanisms for the pathogenesis of LGE. Yet, other mechanisms, such as subclinical myocarditis, vasculitis, or cardiomyopathy19 as well as coronary vasospasm or anomalies including myocardial bridging5 may also have been involved in its development in some athletes, even though marathon runners with any known current or previous CVD were excluded from this study. Further, the HNRS cohort did not undergo CMR scanning at baseline investigation, which precludes a comparison of the prevalence of LGE among these cohorts.
Two events were revascularizations and were in part subject to surveillance bias. The significant stenoses in runners free of symptoms may have been missed outside this prospective study. Even though statistically significant, our event data should therefore be interpreted with caution and longer follow-up in larger cohorts is required. Ideally, event rates in marathon runners should be compared with those in the control groups. However, outcome data from the HNRS will only be available in 2009. Our findings are in a similar magnitude, though, as previously reported from other asymptomatic low-risk cohorts and are in line with existing evidence on the prognostic value of CAC.13
Conclusions
Regular marathon running has a beneficial effect on the cardiovascular risk factor profile but the extent of calcified coronary plaque is underestimated from that risk factor profile, with 36% of marathon runners aged ≥50 having a CAC score ≥100 and 9% of these requiring coronary revascularization during two years of follow-up. Advanced CAC scores seem to contribute to increased myocardial damage and appear to impair outcome. Frequent marathon running may not protect these athletes from the risk of coronary events.
Funding
The Marathon Study was funded by the Ruhrkohle AG (RAG), Essen, Germany. The Heinz Nixdorf Recall Study was funded by the Heinz Nixdorf Stiftung (chairman: Dr. jur. G. Schmidt), Essen, Germany.
Acknowledgements
The authors are indebted to the Ruhrkohle AG (RAG), Essen, Germany for their grant for the Marathon study. We thank the Heinz Nixdorf Stiftung (Dr. jur. G. Schmidt) for the generous support of the HNRS. We thank the HNRS investigative group and gratefully acknowledge the collaboration with Prof. Grönemeyer, Prof. Seibel, and Volbracht. The authors highly appreciate the help of David Kiefer, Martin Hensel, and Mareike Perrey in acquiring data for the Marathon study, and the dedicated personnel both in the HNRS study centre and in the EBT scanner facilities.
By George Borjas Labor Economics(text only)4th (Fourth) edition[Hardcover]2007 2007. By by George Borjas. $59.11 $ 59 11. Only 2 left in stock - order soon. By George Borjas: Labor Economics Fifth (5th) Edition Jan 23, 2009. $152.24 $ 152 24. Only 2 left in stock - order soon. More Buying Choices. $9.86 (51 used & new. George Borjas’ well-received text blends coverage of traditional topics with modern theory and developments into a superb Labor Economics book. The Fourth Edition builds on the features and concepts that made the first three editions successful, updating and adding new content to keep the text on the cusp of recent events in the Labor. Labor Economics - George Borjas. Labor Economics - George Borjas. Jacksom Peter. Download with Google Download with Facebook or download with email. Labor Economics - George Borjas. Labor Economics - George Borjas. Economics borjas 4th edition pdf.
Conflict of interest: none declared.
References
Framingham Risk Calculator
)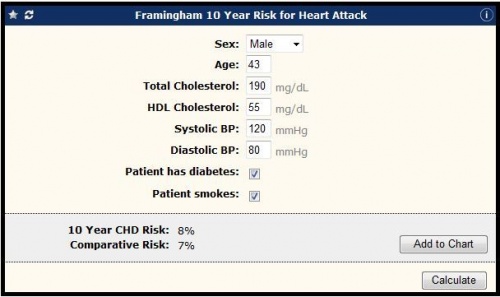

![Jmp statistical discovery 9.0 cracked [jhnm]](http://image.slidesharecdn.com/seriales-100902064725-phpapp01/95/seriales-13-728.jpg?cb=1283410084)